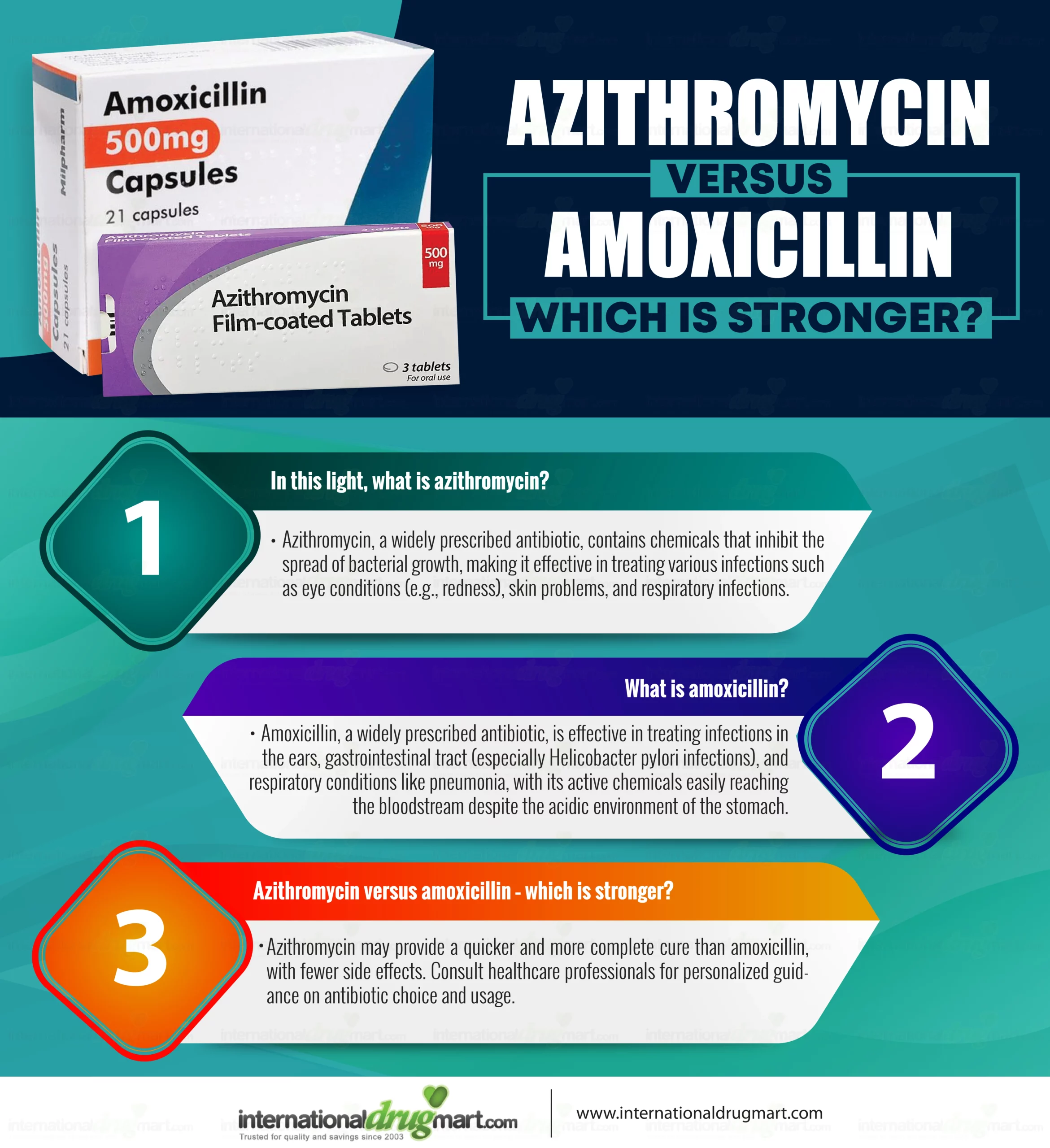
Need an antibiotic stronger than amoxicillin? Consider azithromycin for its broader spectrum against various bacterial infections, particularly respiratory and skin infections. It offers a convenient once-daily dosage, improving adherence.
For serious infections unresponsive to amoxicillin, levofloxacin provides potent activity against gram-negative bacteria commonly causing urinary tract infections and pneumonia. However, remember that fluoroquinolones, such as levofloxacin, carry a higher risk of side effects, so discuss them with your doctor.
Cefuroxime axetil is another excellent alternative with a wide range of activity against both gram-positive and gram-negative bacteria. This makes it suitable for a wider variety of infections compared to amoxicillin. Its oral administration offers convenience, while its intravenous form is effective for severe cases.
Important Note: This information is for educational purposes only. Always consult a healthcare professional before starting any antibiotic treatment. They can accurately diagnose your infection and prescribe the most appropriate and safest antibiotic for your specific needs, considering factors like allergies and resistance patterns.
- Antibiotics Stronger Than Amoxicillin
- Understanding Amoxicillin’s Limitations
- Spectrum of Activity
- Resistance Concerns
- Side Effects
- Alternative Treatment Considerations
- Conclusion
- Cephalosporins: A Broader Spectrum of Action
- Fluoroquinolones: Powerful but with Potential Side Effects
- Carbapenems: Reserved for Serious Infections
- When to Consider Carbapenems
- Understanding the Risks
- Glycopeptides: Fighting Resistant Bacteria
- Choosing the Right Antibiotic: Doctor’s Role
- Antibiotic Resistance: The Growing Threat
- Understanding the Problem
- Combating Resistance
- Preventing the Spread of Resistant Bacteria
- Exploring New Antibiotic Development
- Targeting Bacterial Virulence Factors
- Harnessing Phage Therapy
- Developing Novel Antibiotic Classes
- Improving Diagnostics and Stewardship
Antibiotics Stronger Than Amoxicillin
Amoxicillin treats many bacterial infections, but stronger antibiotics exist for more resistant bacteria. Consider these alternatives:
Cefuroxime: This cephalosporin treats respiratory and skin infections, often effective when amoxicillin fails. It’s generally better tolerated than some stronger options.
Ceftazidime: A potent cephalosporin used for serious infections, particularly those involving Gram-negative bacteria. Hospital use is common due to its strength.
Levofloxacin: A fluoroquinolone, effective against a broad range of bacteria including those resistant to amoxicillin. Side effects, such as tendon damage, need monitoring.
Piperacillin-tazobactam: This combination antibiotic is particularly strong against serious, hospital-acquired infections. It’s a powerful option for severe cases.
Imipenem: A carbapenem, reserved for severe, life-threatening infections resistant to other antibiotics. Its use is often monitored closely due to potential side effects.
Always consult a doctor. Choosing the right antibiotic depends on the specific infection, its severity, and your individual health. Never self-medicate.
Understanding Amoxicillin’s Limitations
Amoxicillin, while effective against many bacterial infections, doesn’t conquer all. Its effectiveness hinges on the specific bacteria causing the infection and their susceptibility to the antibiotic. Many bacteria have developed resistance, rendering amoxicillin ineffective.
Spectrum of Activity
Amoxicillin primarily targets Gram-positive bacteria like Streptococcus and Staphylococcus (though resistance is increasing). It’s less effective against Gram-negative bacteria such as E. coli and Pseudomonas aeruginosa. This limited spectrum means it fails against numerous bacterial infections.
Resistance Concerns
Overuse contributes significantly to amoxicillin resistance. Bacteria adapt, making the antibiotic less powerful over time. Infections previously treatable with amoxicillin now require stronger alternatives. This resistance is a growing global health concern.
Side Effects
Amoxicillin, like any medication, carries potential side effects. Common issues include diarrhea, nausea, and rash. Severe allergic reactions, though rare, can be life-threatening. These side effects necessitate careful monitoring and informed use.
Alternative Treatment Considerations
| Infection Type | Possible Alternatives to Amoxicillin |
|---|---|
| Severe respiratory infections | Levofloxacin, Ceftriaxone |
| Skin infections | Clindamycin, Doxycycline |
| Urinary tract infections | Ciprofloxacin, Nitrofurantoin |
The choice of antibiotic depends on the identified bacteria and the severity of infection. A doctor’s guidance is crucial for selecting the right treatment.
Conclusion
Amoxicillin remains a valuable antibiotic, but its limitations regarding bacterial resistance and spectrum of activity require careful consideration. Consulting a healthcare professional is vital for appropriate diagnosis and treatment choices to ensure optimal patient outcomes.
Cephalosporins: A Broader Spectrum of Action
Cephalosporins often outperform amoxicillin because they target a wider range of bacteria. This broader spectrum stems from their unique chemical structure, allowing them to penetrate bacterial cell walls more effectively than amoxicillin.
Several cephalosporin generations exist, each with increasing resistance to beta-lactamases – enzymes produced by bacteria to break down antibiotics like amoxicillin. First-generation cephalosporins like cefazolin are effective against Gram-positive bacteria. Second-generation cephalosporins, such as cefuroxime, expand this coverage to include some Gram-negative bacteria. Third-generation cephalosporins, like ceftriaxone, further broaden the spectrum, addressing many serious infections caused by both Gram-positive and Gram-negative bacteria. Fourth and fifth-generation cephalosporins offer even greater resistance to beta-lactamases and improved activity against specific bacterial strains.
Specific examples of infections where cephalosporins might be preferred over amoxicillin include: serious respiratory infections, complicated urinary tract infections, and certain types of skin infections. However, always consult a doctor; the choice of antibiotic depends on numerous factors, including the specific bacteria involved, patient’s medical history, and potential drug interactions.
Remember that cephalosporins, like all antibiotics, can have side effects. Common side effects include diarrhea, nausea, and rash. Allergic reactions, though uncommon, are possible. Discuss potential risks and benefits with your physician before using any cephalosporin.
Fluoroquinolones: Powerful but with Potential Side Effects
Fluoroquinolones, like ciprofloxacin and levofloxacin, treat severe bacterial infections where amoxicillin isn’t strong enough. They target a different bacterial enzyme, offering a powerful alternative.
However, these drugs carry a risk of serious side effects. Tendon rupture is a significant concern, especially in older adults or those using corticosteroids. Avoid strenuous activity during treatment.
Peripheral neuropathy, characterized by numbness, tingling, or pain in the hands and feet, is another potential complication. This can be persistent even after treatment ends.
Gastrointestinal issues such as nausea, diarrhea, and vomiting are common, but usually mild. Severe cases, including Clostridium difficile infection, are possible.
Central nervous system effects such as dizziness, headache, and confusion may occur. Avoid driving or operating machinery if experiencing these symptoms.
Prolonged QT interval, potentially leading to irregular heartbeats, is a risk in some individuals, particularly those with pre-existing heart conditions. Your doctor should assess your risk factors.
Before starting fluoroquinolone treatment, discuss potential benefits and risks thoroughly with your doctor. They can help determine if these powerful antibiotics are the right choice for you, considering your individual health profile and the severity of your infection.
Carbapenems: Reserved for Serious Infections
Carbapenems are powerful antibiotics, significantly stronger than amoxicillin. However, their potent nature means they’re reserved for treating serious bacterial infections that haven’t responded to other antibiotics.
When to Consider Carbapenems
- Life-threatening infections: Sepsis, meningitis, pneumonia unresponsive to other treatments.
- Multi-drug resistant bacteria: Infections caused by bacteria resistant to multiple antibiotic classes.
- Intractable infections: Infections that haven’t improved with other antibiotics despite appropriate treatment.
Doctors carefully consider the patient’s condition, the severity of the infection, and the specific bacteria involved before prescribing carbapenems.
Understanding the Risks
- Increased risk of side effects: Carbapenems can cause diarrhea, nausea, vomiting, and allergic reactions.
- Development of resistance: Overuse of carbapenems fuels the development of carbapenem-resistant bacteria, a serious public health concern. Careful prescription is key to preventing this.
- Complex administration: These antibiotics are often administered intravenously or intramuscularly, requiring medical supervision.
Always follow your doctor’s instructions meticulously. Improper use can lead to treatment failure and increase the risk of complications. Discuss any concerns about your medication with your healthcare provider.
Glycopeptides: Fighting Resistant Bacteria
Glycopeptides, like vancomycin and teicoplanin, represent a powerful class of antibiotics effective against Gram-positive bacteria, including those resistant to other antibiotics such as amoxicillin. These drugs target bacterial cell wall synthesis, a process crucial for bacterial survival.
Consider these key points:
- Mechanism of Action: Glycopeptides bind to peptidoglycan precursors, preventing their incorporation into the bacterial cell wall. This leads to cell wall weakening and ultimately, bacterial death.
- Spectrum of Activity: They are particularly useful against methicillin-resistant Staphylococcus aureus (MRSA) and vancomycin-resistant enterococci (VRE), although resistance is emerging.
- Administration: Glycopeptides are typically administered intravenously due to poor oral absorption.
However, using glycopeptides responsibly is vital to prevent resistance. Here are some guidelines:
- Appropriate Use: Reserve glycopeptides for infections caused by bacteria proven or highly suspected to be resistant to other antibiotics.
- Dosage and Duration: Follow prescribed dosage and treatment duration precisely. Incomplete treatment can contribute to resistance development.
- Monitoring: Regularly monitor patients for adverse effects, including nephrotoxicity and ototoxicity. Kidney and hearing function tests may be required.
- Infection Control: Practice rigorous infection control measures to minimize the spread of resistant bacteria in healthcare settings.
While glycopeptides offer a valuable tool in fighting resistant bacteria, responsible usage is paramount to maintain their efficacy. Always consult with a healthcare professional for diagnosis and treatment of bacterial infections.
Choosing the Right Antibiotic: Doctor’s Role
Always consult your doctor before taking any antibiotic, even if you think you know what you need. They will perform a thorough examination and possibly order tests.
Your doctor will consider several factors:
- Your specific symptoms: A detailed description helps pinpoint the likely infection.
- Type of infection: Bacterial, viral, or fungal infections require different treatments. Antibiotics only work against bacterial infections.
- Severity of infection: A mild infection might respond to a common antibiotic like amoxicillin, while a severe infection may need stronger medication.
- Your medical history: Allergies, other health conditions, and current medications influence antibiotic selection to prevent adverse reactions.
- Antibiotic resistance: Your doctor considers local antibiotic resistance patterns to choose the most effective option.
- Pregnancy or breastfeeding: Certain antibiotics are safer than others during pregnancy or while breastfeeding.
Following your doctor’s prescribed dosage and duration is crucial for successful treatment and preventing resistance. Do not stop taking antibiotics prematurely, even if you feel better.
Your doctor will monitor your progress and may adjust your treatment plan if needed. They will also provide guidance on managing side effects.
- Testing: Blood tests, urine tests, or cultures may be performed to identify the specific bacteria causing the infection and its susceptibility to different antibiotics.
- Discussion: They’ll explain the chosen antibiotic, its potential side effects, and what to expect during treatment. Ask questions!
- Follow-up: Schedule a follow-up appointment to assess treatment effectiveness and address any concerns.
Remember: Self-treating with antibiotics is dangerous and can lead to antibiotic resistance. A doctor’s expertise ensures you receive the right treatment for your specific needs.
Antibiotic Resistance: The Growing Threat
The overuse of antibiotics fuels the development of resistant bacteria. This means common infections become harder, sometimes impossible, to treat. The CDC reports that over 2.8 million antibiotic-resistant infections occur annually in the US, resulting in over 35,000 deaths. Globally, the World Health Organization estimates that antimicrobial resistance (AMR) already claims 700,000 lives yearly and projects this number to rise to 10 million deaths by 2050 without significant changes.
Understanding the Problem
Bacteria adapt, developing mechanisms to survive antibiotic exposure. This resistance spreads rapidly through different bacterial strains, creating “superbugs.” Improper antibiotic use, including incomplete courses and use for viral infections, accelerates this process. Factors like sanitation levels and access to healthcare also contribute.
Combating Resistance
Preventing resistance requires a multi-pronged approach. Doctors need to prescribe antibiotics judiciously, only when absolutely necessary. Patients must complete their prescribed courses fully. Public health initiatives focused on hygiene and sanitation are crucial. Investing in research to develop new antibiotics and alternative therapies is also vital. We must act now to protect our future health.
Preventing the Spread of Resistant Bacteria
Finish all prescribed antibiotics. Don’t stop taking them early, even if you feel better. This ensures all bacteria are eliminated, reducing the chance of resistance developing.
Practice meticulous hand hygiene. Wash your hands thoroughly with soap and water for at least 20 seconds, especially after using the restroom and before eating. Use an alcohol-based hand sanitizer when soap and water aren’t available.
Avoid sharing personal items. This includes towels, razors, and toothbrushes. These items can easily spread bacteria.
Cook food to the proper internal temperature. Improperly cooked food can harbor harmful bacteria. Use a food thermometer to ensure meats are cooked thoroughly.
Practice safe sex. Sexually transmitted infections can contribute to antibiotic resistance. Use barrier methods like condoms.
Get vaccinated. Vaccines protect against many bacterial infections, reducing the need for antibiotics.
Clean and disinfect surfaces regularly. Focus on frequently touched areas like doorknobs, light switches, and countertops. Use disinfectants proven to kill bacteria.
| Action | Impact |
|---|---|
| Complete antibiotic courses | Reduces bacterial survival and resistance development. |
| Improved hygiene | Minimizes bacterial transmission. |
| Safe food handling | Prevents bacterial contamination and infection. |
| Safe sex practices | Reduces STI transmission and antibiotic use. |
| Vaccination | Provides immunity against bacterial infections. |
| Surface disinfection | Eliminates bacteria in high-traffic areas. |
Consult your doctor before using antibiotics. Antibiotics are powerful medicines and should only be used when necessary. Misuse contributes to resistance.
Exploring New Antibiotic Development
Scientists are actively pursuing several promising avenues. One key strategy focuses on modifying existing antibiotics to circumvent bacterial resistance mechanisms. This involves altering the antibiotic’s structure to improve its ability to penetrate bacterial cells or inhibit resistance enzymes.
Targeting Bacterial Virulence Factors
Instead of directly killing bacteria, researchers are exploring drugs that target bacterial virulence factors–the molecules that contribute to bacterial disease. Disrupting these factors can weaken the bacteria’s ability to cause infection, reducing the need for potent antibiotics and lessening the selective pressure that drives resistance. This approach holds significant potential for tackling infections caused by resistant strains.
Harnessing Phage Therapy
Bacteriophages–viruses that infect and kill bacteria–offer a novel approach. Phage therapy involves using phages to specifically target and destroy pathogenic bacteria. Research is ongoing to refine phage cocktails and delivery methods for effective treatment of bacterial infections. Personalized phage therapy, tailored to individual patients and their specific bacterial infections, is also being investigated.
Developing Novel Antibiotic Classes
Researchers are actively searching for entirely new classes of antibiotics. This involves screening diverse natural sources, such as soil samples and marine organisms, for novel antibiotic compounds. Sophisticated high-throughput screening techniques are used to identify promising candidates. Synthetic biology is also being employed to design and create novel antibiotic structures with improved activity and reduced toxicity. These efforts may yield antibiotics that overcome existing resistance mechanisms.
Improving Diagnostics and Stewardship
Faster and more accurate diagnostics are critical for selecting the right antibiotic and limiting unnecessary use. Rapid diagnostic tests can significantly shorten treatment times and improve patient outcomes. Responsible antibiotic stewardship programs – promoting appropriate prescribing practices and limiting unnecessary antibiotic use – are also vital in delaying the emergence of antibiotic resistance.